Hypertension – Care Heart for a Healthy Life
This content has been Medically reviewed by Dr. Amol Kamalakar Pathak, MBBS, MD (MEDICINE), DNB (MEDICINE), MNAMS
Introduction
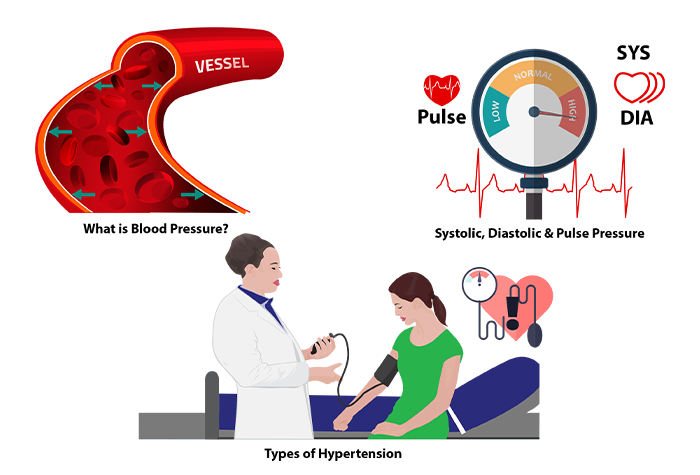 What is Blood Pressure?
What is Blood Pressure?
Blood Pressure is the force that a person’s blood exerts against the walls of their blood vessels. This pressure depends on the resistance of the blood vessels and how hard the heart has to work.
As the heart pushes the blood into the arterial system on a single stroke, two pressures are important. Systolic or higher pressure is the force generated when the blood is pushed into the arteries. Diastolic or lower pressure when the heart relaxes to fill with blood as it gets ready for the next push.
Definition of Hypertension
Hypertension (or HTN) or high blood pressure is defined as abnormally high arterial blood pressure. Normal adult blood pressure, on average, is 120 systolic and 80 or less diastolic, usually expressed as 120 over 80. Individually, the numbers correspond to millimeters of mercury,this is expressed in fraction as 120/80. If the values of systolic/diastolic BP exceed 140/90mmHg on repeated determination it is likely that one may be suffering from hypertension.
Systolic, Diastolic, and Pulse Pressure
Systolic BP
It’s the maximum pressure exerted on the blood vessels by the blood when the heart contracts. It’s approximately 120mm Hg.
Diastolic BP
It’s the minimum pressure experienced when the heart is relaxing. Its approximate value is 80mm Hg. Normally, systolic blood pressure rises through the adult age range, whereas diastolic blood pressure peaks at about age 60 in men and 70 in women, and falls gradually thereafter.
Pulse Pressure: It’s the difference between systolic and diastolic BP.
Pulse Pressure = Systolic BP – Diastolic BP.
Normal Pulse Pressure is approximately 40mm Hg.
Primary or Essential hypertension
If any individual notices high blood pressure frequently on three or more visits and eliminates other causes of hypertension, one may be suffering from essential or primary hypertension. There are no specific symptoms but a person may experience few symptoms such as frequent headaches, tiredness, dizziness or nose bleeds.
It has no clear underlying cause but appears to be the result of an interplay of combined complex factors such as heredity, excess weight, poor diet, and lack of fitness, to name a few. 97-98% of the population are induced to it.
Secondary Hypertension
It is a result of various other secondary causes. One of the causal factors is renovascular disease (kidney diseases). Other underlying causal factors include obstructive sleep apnea (snoring, daytime sleepiness, morning headache, irritability), and primary aldosteronism (fatigue, constipation, polyuria, polydipsia). Drugs that can also cause secondary hypertension may include over-the-counter medications such as ibuprofen (Motrin, Advil, and others) and pseudoephedrine (Afrin, Sudafed, and others).
2-5% of the population usually suffer from it. Hence, secondary hypertension is usually referred to as a byproduct of other illnesses. It has been observed that 10% of patients with primary hypertension are prone to secondary hypertension.
Isolated Systolic Hypertension (ISH)
The term isolated systolic hypertension (ISH) has particular relevance to elderly subjects. With isolated systolic hypertension, the systolic pressure rises above 140mm Hg, while the lower number stays near the normal range, below 90. There is a loss of elasticity in the arteries. As per research, it has been observed that systolic pressure is much more important than the diastolic pressure when it comes to the risk of cardiovascular disease for an older person.
According to the National Health and Nutrition Examination Survey (NHANES), ISH is the most prevalent type of untreated hypertension over 60 years of age. ISH represents a substantial health care problem as the target BP is very difficult to attain by drug therapy.
Malignant Hypertension
Malignant hypertension (MHT), also known as accelerated-malignant hypertension or malignant-phase hypertension, is the most severe form of hypertension; it is defined clinically as high blood pressure (BP) where diastolic pressure goes over 130mm Hg. It is extremely high blood pressure and should be treated as a medical emergency. Symptoms include numbness in the arms and legs, blurred vision, confusion, chest pain, and headache.
It may result in multiple organ damage. About 1% of people with hypertension are prone to this form of hypertension. It is more common in younger adults, African-American men, and women who have pregnancy toxemia.
Resistant Hypertension
Resistant hypertension (RH) is defined as above-goal elevated blood pressure (BP). In this condition, blood pressure levels are <140/90mmHg for the general population and <140/85mmHg for patients with diabetes and chronic kidney disease.
In this condition despite the concurrent use of 3 antihypertensive drug classes, commonly including a long-acting calcium channel blocker, a blocker of the renin-angiotensin system (angiotensin-converting enzyme inhibitor or angiotensin receptor blocker), and diuretics, BP is not in the normal range. 12%-18% of hypertensive patients suffer from resistant hypertension. This form necessitates a detailed historical, clinical, and investigative analysis.
Classification of Hypertension
| Category | Systolic Blood Pressure (mmHg) | Diastolic Blood Pressure (mmHg) | |
|---|---|---|---|
| Optimal | < 120 | and | < 80 |
| Normal | 120-129 | and/or | 80-84 |
| High Normal | 130-139 | and/or | 85-89 |
| Grade 1 Hypertension | 140-159 | and/or | 90-99 |
| Grade 2 Hypertension | 160-179 | and/or | 100-109 |
| Grade 3 Hypertension | ≥ 180 | and/or | ≥ 110 |
| Isolated Systolic Hypertension | ≥ 140 | and | < 90 |
| Malignant Hypertension | > 200 | and | > 120 |
Hypertensive Crisis
Hypertensive crisis is defined as a severe elevation in blood pressure (> 180/120 mm Hg). Immediate treatment of hypertension in this setting is mandatory, if untreated it may lead to organ failure.
Hypertensive crisis are subdivided into hypertensive emergencies and urgencies.
Hypertensive Urgency
In this condition, BP shoots up and it needs to be lowered within 24-48 hours to prevent the development of acute organ damage. Symptoms like headache, dizziness, severe anxiety, epistaxis and shortness of breath are experienced. Hypertensive urgency is managed using oral antihypertensive drugs in outpatient or same-day observational settings.
Hypertensive Emergency
Diagnosis of hypertensive emergency requires a thorough history (evidence of target organ damage, illicit drug use, and medication compliance), a complete physical examination, basic laboratory data, and electrocardiogram data to assess the presence of target organ damage and determine its severity. Hypertensive emergency is managed in an intensive care unit or other monitored settings with parenteral drugs.
How Prevalent is Hypertension?
Globally: Around 7.5 million deaths or 12.8% of all the deaths, every year, worldwide
occur due to high blood pressure. It is predicted that 1.56 billion adults will have hypertension by 2025. According to WHO 13 % of deaths globally are due to high blood pressure.
National: It was observed that hypertension prevalence varied from 2-15% in urban India and 2-8% in rural India in the late nineties to early twentieth century. The epidemiological studies prove that hypertension has increased in both urban and rural subjects from 10-15% to 25% .
It has been observed that the burden of hypertension among the elderly population in the Indian subcontinent is on the rise.
 Diagnosis and Screening for Hypertension
Diagnosis and Screening for Hypertension
As mentioned in the literature, uncomplicated (primary) hypertension is usually asymptomatic and many of the symptoms often related to hypertension are mostly psychogenic in origin.
Hypertension rarely causes symptoms in the early stages and many people go undiagnosed.
General Signs and Symptoms associated are
- Headaches, especially in the morning
- Ringing in the ears
- Unexplained dizziness
- Spontaneous nosebleeds
- Depression without apparent cause
- Blurred vision
- Tension when there is no cause
- Flushing of the face
- Fainting spells
Weight, BMI and Waist Circumference
BMI is the most appropriate simple indicator where weight-for-height ratio can be related to health outcomes. WHO (1995) therefore proposed the use of BMI to monitor both undernutrition and overweight.
Measurement of waist circumference is an indicator of the quantity of abdominal fat, which correlates with the amount of intra-abdominal or visceral fat. An excess of abdominal fat has been associated with a range of metabolic abnormalities and diseases. Various studies have shown that an increase in body mass index as well as an increase in age are linked to rising blood pressure and can lead to hypertension.
Comparing BP on both Arms
Blood pressure (BP) is characterized by large spontaneous variations, therefore the diagnosis of hypertension should be based on multiple BP measurements taken on several separate occasions. Measurement of blood pressure outside the clinic may provide valuable information for the initial evaluation of individuals with hypertension and for monitoring the response to treatment.
Home measurement has the advantage that it distinguishes sustained hypertension from “white-coat hypertension”, a condition noted in patients whose blood pressure is elevated in the physician’s clinic but normal at other times. For home blood pressure, readings of more than 135/85 mm Hg should be considered elevated.
Theoretically measuring BP on both arms is a simple and quick task. It may be helpful to assess vascular diseases. In the market, there are various devices for measuring blood pressure, such as
- Manual sphygmomanometers,
- Digital non-portable for an upper arm with automatic inflation
- Digital portable for an upper arm with automatic inflation,
- Digital portable for wrist with automatic inflation
- Digital portable for fingers with automatic inflation.
The patient is always recommended to consult their physician before going to any conclusions regarding the blood pressure measures.
The American Heart Association (AHA) has listed 7 common mistakes that may result in erroneously high BP measurement and inaccurate diagnosis of hypertension. (AHA, April 30, 2018)
These include
- Having a full bladder : Can add 10-15 points to the reading.
- Slouching, unsupported back or feet: Sitting with no support to back or feet can increase the BP reading by 6-10points. Make sure to sit in a chair with back support and have feet flat on the floor or a footstool.
- Unsupported arm: While measuring BP, the arm should be placed on a table or flat counter, so that the measurement cuff is level with the heart. The BP reading increases by up to 10 points if the arm is hanging by the side or if it has to be held up to see the reading.
- Sitting with crossed legs: It may increase blood pressure reading by 2-8 points.
- Wrapping the cuff over clothing: Increases reading by 5-50 points to the reading. So, the cuff should be applied over a bare arm with right sized cuffs.
- Using too-small a cuff : This may increase reading by 2-10 points. Select the right size when measuring BP.
- Answering questions or talking on the phone: It may add 10 points to the measured BP reading. Stay still and silent while the BP is being measured.
Other Tests Recommended for Hypertension
These tests are recommended for secondary hypertension to check for other complications associated with it.
Cholesterol
High blood cholesterol itself does not cause symptoms, so many people are unaware that their cholesterol level is too high. So it is a must to find out what your cholesterol numbers are. A blood test called a ‘lipoprotein profile or lipid profile’ gives your cholesterol numbers. It gives clear information about total cholesterol, LDL (bad) cholesterol, HDL (good) cholesterol and triglycerides levels in the blood.
ECG
An electrocardiogram (ECG) is a test that measures the electrical activity of your heart. An electrocardiogram can be a useful way to find out whether your high blood pressure has caused any damage to your heart or blood vessels. Because of this, you may be asked to have an ECG when you are first diagnosed with high blood pressure. Hypertensive cardiac damage is also identified by left ventricular hypertrophy (LVH).
Sodium and Potassium
Blood electrolyte levels are very important in hypertension. Electrolyte imbalances are more common in older people and individuals with comorbid conditions. High blood pressure results from many factors, excessive salt and an incorrect balance between sodium and potassium may be considered as one of the risk factors as there are relationships between dietary potassium and sodium and hypertension.
Serum potassium or sodium is usually measured. Usually, medical care is recommended for patients with serum sodium < 120 mmol/L or > 150 mmol/L, or rapidly decreasing or increasing levels. Patients with serum potassium ≤ 2.5 mmol/L or ≥ 7 mmol/L, rapidly decreasing or increasing levels also need to seek medical attention.
Uric Acid
Elevated levels of uric acid in serum is termed as hyperuricemia. Serum uric acid (SUA) is the end product of purine metabolism; its overproduction and decreased excretion via kidneys usually result in hyperuricemia. There is mostly an association between serum uric acid levels and hypertension. Elevated levels of uric acid may indicate the onset of essential hypertension in adolescents and prehypertension. Individuals with serum uric acid levels >416.4 µmol/L (7.0 mg/dL) in men and >356.9 µmol/L (6.0 mg/dL) in women can be categorized as hyperuricemia.
Albumin
Albumin is a vital protein normally present in the blood. There should be a complete absence of this protein in urine if the kidneys are functioning properly. The hypothesis is that high urinary albumin excretion (UAE) usually indicates mild renal damage. UAE is associated with Glomerular Filtration Rate (GFR) and is usually a primary indication of the development of hypertension. Urinary albumin may be an indication of the development of hypertension and future increases in blood pressure in the normotensive general population. Microalbuminuria is defined as levels of albumin ranging from 30 to 300 mg in a 24-h urine collection. Microalbuminuria or proteinuria is defined as a urinary albumin excretion of ≥300 mg/24 h.
Various Causes of Hypertension
 Genetics and Family History
Genetics and Family History
Hypertension has long been recognized as a condition that affects one’s well-being. It has long been known that hypertension involves a genetic component. Although several genes based on familial cases have been identified, majority of obese individuals occur randomly in the population.It is usually found that hypertension is hereditary. If you have someone in your family (a blood relative such as a mother, father, sister, or brother) who has or had high blood pressure before the age of 60, a higher likeliness of developing hypertension has been observed.
Age and Gender
Blood pressure increases with age in both genders. It rises more in those with higher initial BP. Men display a higher average BP. Probability of having hypertension increases after menopause in women. Men are at greater risk for cardiovascular and renal disease than are age-matched, premenopausal women. Recent studies using the 24-hour ambulatory blood pressure monitoring technique have shown that blood pressure is higher in men than in women at similar ages.
After menopause, however, blood pressure increases in women to levels even higher than in men. Studies show that men are more prone to hypertension below the age of 50. After the age of 50, women are at a higher risk for the disease because of menopause. Men have a greater blood pressure load on the organs when affected by hypertension as compared to women.
Obesity
Various studies show that an increase in BMI is linked to rising BP and ultimately to hypertension. It has been observed that obesity impairs carbohydrate metabolism. A more common cause of high blood pressure in overweight people is excess insulin. Because fat cells are less sensitive to insulin in some overweight people, their bodies produce more insulin, and extra insulin signals the kidneys to increase blood pressure.
Obesity is associated with increased visceral adiposity and is a major cause of hypertension, accounting for 65% to 75% of the risk of primary (essential) hypertension. Increased renal tubular sodium reabsorption impairs pressure natriuresis and plays an important role in initiating obesity hypertension.
Dietary Habits
Dietary habits may contribute substantially to the development of weight gain ultimately resulting in hypertension. Dietary factors that can cause hypertension are excess consumption of salt (sodium) with low intake of potassium, calcium, and magnesium. High Consumption of processed foods that are rich in salt, energy-dense food and drinks, and low fiber diet may cause hypertension.
Diabetes (Type 2 Diabetes Mellitus)
Diabetes is often a contributor to the development of high blood pressure in elderly people. Poor diet and high sugar intake can aid the development of diabetes and the incidence of the disease increases with age. It has been observed that in more than 50% of individuals with T2DM, hypertension is more prevalent. The presence of hypertension in patients with diabetes markedly enhances the development of macrovascular and microvascular disease in these individuals. Diabetic individuals with coexisting hypertension have a much greater prevalence of stroke and transient ischemic episodes than normotensive diabetics.
Lifestyle Changes
A sedentary lifestyle also appears to be associated with hypertension. Work-related activity has declined over recent decades in industrialized countries due to modernization, convenient services, and high standard of living. These lead to insufficient physical activity, as most of them do not engage in regular aerobic exercise and are at increased risk of developing hypertension. Along with this, excessive alcohol consumption, tobacco/caffeine intake, and irregular sleep patterns are considered important risk factors for hypertension.
Drug-Induced
Many prescription and nonprescription drugs can cause or exacerbate hypertension. Some of the drug classesare, Immunosuppressive agents (Cyclosporine), NSAID (Naproxen), Hormonal Medicines (Estrogen Oral Contraceptives), Stimulants (Nicotine), Anabolic Steroids (Testosterone), and Antiparkinsonian (Bromocriptine).
Sleep Disorders
Sleep deficiency is becoming widespread in both adults and adolescents. This disorder occurs in 2%-4% of adult populations worldwide and out of which 50% have hypertension. The index is usually higher in any hypertensive patient whose BMI is above the normal range leading to obesity.
Various studies have found that people with shorter sleep duration are more likely to be overweight or obese,which eventually leads to hypertension if untreated. Hence strategies for the management of hypertension should be incorporated considering sleep patterns. Confirmation of the diagnosis is accomplished by a formal sleep study. The impact of sleep disorder is probably high on the cardiovascular system due to its association with elevated blood pressure.
Psychosocial Stress
The relationship between psychosocial stress and hypertension has been hypothesized. During stress, our body produces stress related hormones which stimulates the heart to beat fast and narrows down the blood vessels, thereby increasing the blood pressure. But stress induced hypertension is temporary and can be controlled easily through lifestyle changes.Stress and long-term high blood pressure may not be linked, but taking steps to reduce your stress can improve your blood pressure including general health.
Complications Associated With Hypertension
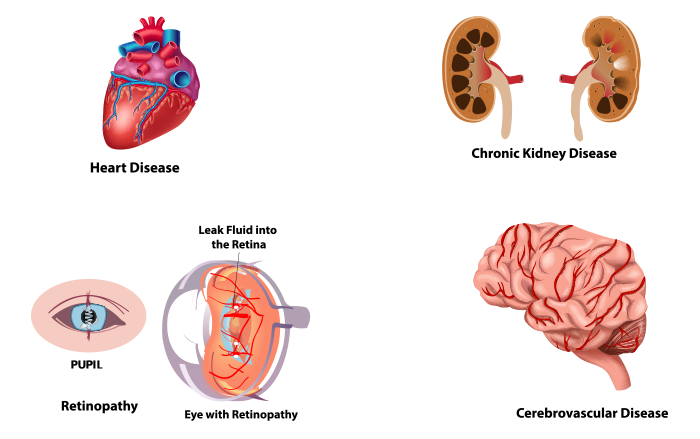 Heart Diseases
Heart Diseases
Coronary artery disease is associated with, and accelerated by, chronic arterial hypertension. Which may lead to myocardial ischemia and myocardial infarction. Indeed, myocardial ischemia is much more frequent in untreated or poorly controlled hypertensive patients than in normotensive patients. Two main factors contributing to myocardial ischemia are, a pressure-related increase in oxygen demand, and a decrease in coronary oxygen supply resulting from associated atheromatous lesions.
Cerebrovascular Diseases
Cerebrovascular disease is a group of conditions, diseases, and disorders that mostly affect the blood vessels and blood supply to the brain. Chronic arterial hypertension is the most significant modifiable risk factor for stroke (ischemic and hemorrhagic). Treatment of hypertension results in lower cardiovascular morbidity and mortality, including that due to stroke. Chronic hypertension is an important cause of vascular pathology, which leads to stroke and intracerebral hemorrhage.
Chronic Kidney Disease
High blood pressure is a leading cause of Chronic Kidney Disease (CKD). Over time, high blood pressure can damage blood vessels throughout your body. This can reduce the blood supply to important organs such as the kidneys. High blood pressure also damages the tiny filtering units in your kidneys. As a result, the kidneys may stop removing wastes and extra fluid from your blood. The extra fluid in your blood vessels may build up and raise blood pressure even more.
Advanced Retinopathy
In hypertensive condition arteries are less elastic, narrowed and damaged eventually. Hypertensive retinopathy is the result of damage to the blood vessels supplying blood to retina. A fundus (retinal) examination to determine the presence and severity of retinopathy signs has been recommended as a means to determine the presence of end-organ damage in persons with hypertension and to stratify risk. Hypertension is not just a risk marker for retinopathy, the treatment of hypertension is beneficial.
Ways to Control Hypertension
 Healthy Diet
Healthy Diet
Nearly everyone with high blood pressure can dramatically lower their blood pressure by their changes in diet and lifestyle. Emphasizing on foods low in sodium, rich in complex carbohydrates, balanced consumption of saturated fat to unsaturated fat and increasing fiber in your diet may help to maintain a healthy blood pressure. It can be achieved by eating lots of vegetables, grains, and fruits.This means shifting towards a more healthy diet and fewer processed foods.
Adopting the DASH: DASH stands for Dietary Approaches to Stop Hypertension. It is an eating plan that is based on research studies sponsored by the National Heart, Lung, and Blood Institute (NHLBI). These studies showed that DASH lowers high blood pressure and improves levels of cholesterol.
Recommended Servings in the DASH Eating Pattern, by Calorie Level
| Recommended Servings/Day in the DASH Eating Pattern | ||
|---|---|---|
| Food groups | 1600 Calorie/day | 2,000 calories/day |
| Grains and grain products (include at least 3 whole grain foods each day) | 6 | 6 – 8 |
| Fruits | 4 | 4 – 5 |
| Vegetables | 3- 4 | 4 – 5 |
| Fat free or low fat milk and milk products | 2 – 3 | 2 – 3 |
| Lean meats, fish, or poultry | 3-6 | ≤ 6 |
| Nuts, seeds, and legumes | 3 per week | 4 – 5 per week |
| Fats and oil | 2 | 2-3 |
| Sweets and added sugars | 0 | ≤ 5 per week |
Source: National Heart, Lung, and Blood Institute
Physical Exercises
It has been observed that people who exercise regularly have lower blood pressure and are much less likely to develop high blood pressure. Moderate regular exercise strengthens the heart, improves cardiac output, reduces blood pressure, and increases lean body mass.
Efficient cardiac output means the heart pumps more blood with each beat. Aerobic exercises such as walking, running, swimming when done for at least twenty minutes, or even up to an hour daily, can be helpful as they help to tone the entire cardiovascular system, and also efficiently pump blood to the entire body with less pressure.On an average regular aerobic exercise can reduce the blood pressure by 5 to 7 mm Hg in hypertensive individuals
Watch your Alcohol and Caffeine Intake
Alcohol alters the potassium-sodium-calcium-magnesium balance in the fluid within and surrounding the cells. This causes constriction of the capillaries with an increase of the peripheral resistance, and high blood pressure follows. Try to limit the consumption of alcohol to no more than a wine or one mixed drink. If individuals’ elevated blood pressure is alcohol-related, it is wise to stop alcohol intake. Caffeine promotes anxiety and irritability, and may increase central nervous system activity along with a slight rise in pulse.
Reduce the Sodium intake
We are accustomed to more salt, as we need to develop our taste buds for some bland taste. While shopping, be careful with food labels, supermarkets have some low-sodium foods that are becoming more and more rampant. Reabsorption of sodium as sodium chloride can work against us by precipitating diet-related high blood pressure. Most processed and preserved foods contain large quantities of salt, and people often liberally add salt to food. The American Heart Association recommends intake of not more than 2300mg of sodium per day, the ideal range would be 1500 -2300mg per day for healthy adults.One teaspoon of table salt provides 2300mg of sodium, which is equivalent to daily recommended intake of sodium.
Increase Dietary Potassium
The most important factor for high blood pressure is an incorrect balance between sodium and potassium. The ratio of potassium to sodium in our body is critical. Our body maintains a ratio of about three parts potassium to one part sodium. High potassium consumption helps to excrete excess of sodium from the body. Potassium controls blood pressure by reducing the tension on artery walls. The recommended intake of Potassium for adults is 4700mg per day. High potassium intake is harmful for individuals with kidney diseases and certain medications. It is advisable to identify the underlying cause for hypertension and seek advice of health professionals for assistance. Fad diets are usually inadequate in dietary potassium, which may prove harmful if not monitored smartly.
Say No to Smoking
It has been observed that tobacco use increases blood pressure. So anyone that smokes needs to be careful and look out for symptoms. In fact, anyone who has high blood pressure must immediately stop smoking. Smoking is a major risk factor for every type of cardiovascular disease (CVD). High blood pressure is also a major risk factor for heart attack and stroke. When you smoke and have high blood pressure, the combined risks for CVD, heart attack, and stroke increases.
Medications as prescribed
There are two well-established strategies to lower BP; lifestyle interventions such as healthy diet, exercise, lifestyle changes, and drug treatment. About 80 percent of all high blood pressure can be completely controlled by diet, food, and lifestyle. However the drug treatment of hypertension is also important, as recommended by the physician. Various classes of drugs which are included for hypertension treatment are
- Centrally acting alpha agonists
- Beta adrenergic blocking agents
- Angiotensin converting enzyme inhibitors
- Angiotensin II receptor blockers
- Dihydropyridine calcium channel blockers
- Director vasodilators
- Thiazide diuretics
- Loop Diuretics
- Mineralocorticoid receptor blockers
TFI (The Fit Indian) Support
 Dietary Approach
Dietary Approach
TFI Dietary Approach through our Specially Designed Diets and Functional Food. The principle behind the planning of hypertension diet plans includes.
Low Sodium Diet
Sodium plays a very important role in controlling hypertension. High sodium levels in the blood increase the blood pressure. Our nutritionists have planned a diet that includes foods low in sodium naturally, which helps to decrease the high sodium levels in the body.
High Potassium (K+)
Increasing the consumption of potassium through the diet will help reduce high blood pressure.Potassium helps to excrete excess sodium from the body and also reduces the pressure exerted by the blood on the arteries. Foods such as bananas, spinach,dry fruits which are a rich source of potassium are included in the diet.
Polyunsaturated Fatty Acid Foods
Hypertensive individuals are at a high risk of developing cardiovascular disease. In order to prevent further complications of hypertension and to control it, foods rich in polyunsaturated fatty acids are included. PUFA prevents the build up of fat in the arteries which enables \ free circulation of blood without any blockage, thereby controlling the blood pressure.
Proper Hydration
Lack of fluid consumption will accumulate excess sodium in the blood leading to elevated blood pressure levels. Proper hydration with sufficient amount of fluid consumption at the right intervals will help to eliminate excess sodium and other toxins from the body. Fluids can be in the form of fruit or vegetable juices, soups, ORS, buttermilk, lime juice or simply plain water.
Fiber Rich Foods
Inclusion of foods rich in fiber delays the process of digestion and aids in weight loss for obese individuals, which is one of the major causes of hypertension. Inclusion of 25-30gm of fiber daily in the diet will help to prevent other complications frrom hypertension such as diabetes, cardiovascular disease etc.
Weekly Diet Plans
| Week 1 | Week 2 | Week 3 | Week 4 | |
|---|---|---|---|---|
| Early Morning (6:00 AM – 7:00 AM) |
Have 1 glass of Warm Water diluted with 1 tsp of Aloe Vera Juice as soon as wake up. | Have 1-2 glasses of Warm Water as soon as you wake up [AND] After 10 minutes, have 5 to 8 Almonds (soaked overnight and peeled before eating). |
Have 1 glass of Water (stored overnight in copper bottle) [AND] Have 2 tsp of Flax Seed Powder as soon as you wake up. |
Have 1/2 litre of Water diluted with few drops of Lemon Juice as soon as you wake up [AND] Have 2 tbsp of dry fruits and nuts. |
| Approximate Calories | 8 kcal | 50 kcal | 60 kcal | 180 kcal |
| Breakfast (8:00 AM – 10:00 AM) |
Have 3-4 Small Idlis with Green Chutney [AND] Have 4 dates. |
Have 1 cup of Oatmeal with Skimmed Milk topped with Chopped Apple and Walnuts. | Have Moong Dal Chilla with Plain Curd. | Have 2 Toasted Bread with Egg White Spinach Omelette. |
| Approximate Calories | 250 kcal | 300 kcal | 280 kcal | 280 kcal |
| Midmorning (11:00 AM – 12:00 PM) |
Have 1 cup of cut Papaya with 1 tsp of Sunflower Seeds. | Have 1 glass of Buttermilk with 2 tsp of Pumpkin Seeds | Have one full Guava and 2 Walnuts. | Have 1 glass of Watermelon Juice. |
| Approximate Calories | 160 kcal | 160 kcal | 130 kcal | 130 kcal |
| Lunch (12:30 PM to 2:00 PM) |
Have 1 cup of Green Leaf Salad, 1/2 cup of Brown Rice with 1 cup of Dal and Gourd Curry. | Have 1 bowl of Quinoa Sprouts Tomato Salad, 1 Grilled Fish Fillet or 1 cup of low fat Curd. | Have 1 cup of Pomegranate Tofu Salad, 2 Phulkas with 1 cup of Vegetable Curry. | Have 1 cup of Chicken Soup, 1/2 cup of Millet Rice, 1 cup of Vegetable Curry and Few Slices of Cucumber. |
| Approximate Calories | 300 kcal | 300 kcal | 320 kcal | 310 kcal |
| Snack (4:00 PM to 5:00 PM) |
Have 1 cup of Ginger Tea with 2 Digestive Biscuits [AND] After 30 minutes, have 1 fruit of your choice. |
Have 1 cup of Lemon Mint Tea [AND] Have 1 cup of Roasted Makhana. |
Have 1 cup of Tea [AND] Have a handful of Steamed Sprouts. |
Have 1 cup of Green Tea [AND] After 30 minutes, have one Banana. |
| Approximate Calories | 230 kcal | 170 kcal | 130 kcal | 80 kcal |
| Dinner (7:00 PM to 8:30 PM) |
Have 1 cup of Homemade Vegetable Soup, 1 Chapati roll with 1/2 cup of Stir Fried Chicken and Bell Peppers. | Have 1 bowl of Fruit Salad, 1/2 cup of Rice with 1 cup of Dal and few slices of Carrot | Have 1 cup of Sauteed Vegetables, 2 Ragi Roti and 1/2 cup Plain Dal. | Have 2 Methi Chapathi with 1 cup of Chana Curry. |
| Approximate Calories | 280 kcal | 380 kcal | 340 kcal | 320 kcal |
| Bedtime (9:00 PM to 10:00 PM) |
Have 1 cup of Skimmed Milk before going to bed. | Have 1 glass of Water and 2 Dates before going to bed. | Have 1 glass of Buttermilk before going to bed. | Have 1 cup of Skimmed Milk before going to bed. |
| Approximate Calories | 120 kcal | 34 kcal | 120 kcal | 120 kcal |
| Total Calories | 1400 kcal | 1400 kcal | 1400 kcal | 1400 kcal |
Workouts
Aerobics: Regular walking or jogging 5 days a week 30-40minutes is advised. Swimming is also a good option as a hobby and a full-body activity. Swim on an average for 20-30 minutes.
Strength Training: This type of exercise builds muscle, which burns more calories than fat even when you are not exercising. Aim for two to three sessions of strength training weekly, on alternate days.
Stretching: Aim to do stretching exercises at least three times weekly, including before other workouts. Stretching also promotes better circulation.
Supplementary Therapy
Dietary supplements are generally regarded as classes of foods, not drugs. This is because like foods, most dietary supplements are not screened for safety and effectiveness. It has been observed through various studies that patients suffering from hypertension have also shown significant benefits from supplements, herbs, and other alternative therapy used to maintain blood pressure. It is, therefore, a common practice among patients attending a medical care setting to use dietary supplements.
Calcium and Vitamin D3
Adequate calcium intake is positively linked to lower blood pressure. Individuals who consume less than the Recommended Dietary Allowance (RDA) DRI for calcium may consider taking a calcium supplement. Calcium is an important compound to perform muscle contractions and hence help maintain a healthy heart.
Omega 3
Fish oil is a rich source of Omega-3 fatty acids. It reduces cardiometabolic risk factors, prevents sudden cardiac death after myocardial infarction, reduces raised plasma triglycerides, reduces blood pressure and ameliorates atherogenic effects.
Moringa
Moringa is a rich source of Chlorogenic acid. It is an antioxidant in Moringa extract, and can combat inflammation due to oxidative damage. Research suggests that chlorogenic acid can also regulate blood pressure
Wheatgrass
The chlorophyll in wheatgrass has similar properties to human blood cells. When consumed, within our body the chlorophyll increases the blood cell count and more oxygen is supplied to the organs. Wheatgrass may also help to normalise blood pressure.
Noni
Noni is rich in antioxidants which keep cholesterol in check and prevents arteries from getting blocked. It is a great source of potassium, which is needed for the heart to keep beating and pumping blood. It is cardio protective in nature.
Flaxseed Oil
High blood pressure causes extra stress to the heart since it needs to work harder, Flaxseed oil helps lower the blood pressure. High blood pressure also causes the arteries to become less elastic. Flaxseed oil, specifically the Omega-3 fatty acid in it, helps restore the elasticity, further helping the heart stay healthy.
Grape Seed Extract
Inflammation in the arteries can restrict blood flow and lead to blood pressure issues. Antioxidants in grape seed extract can combat this inflammation regulating and maintaining blood pressure.
Conclusions
Hypertension is becoming a common health problem worldwide, and is resulting in decreased life expectancy. It is known as a silent killer as it is usually asymptomatic, though it is simple to diagnose using new approaches and technologies. Various risk factors that may lead to hypertension are genetics and family history, obesity, psychological stress, diabetes, and lifestyle.
It can be controlled through a combination of healthy diet, regular exercise, healthy lifestyle and medication. As untreated hypertension may lead to serious conditions it’s always wise to start the treatment and monitor/maintain a healthy blood pressure. The Fit Indian (TFI) brings you a dietary approach especially designed to keep your blood pressure under control through nutrition support along with physical workout assistance. With honest commitment towards health, one can definitely maintain a healthy blood pressure using TFI support.

( PhD in Bioprocess Technology)
Her research interests are biosurfactants, pharma biotech, food sciences, analytical chemistry with five international publications in peer-reviewed journals. Awarded research fellowship DBT- India (2007-2009) and UGC-SAP- Delhi India (2009-2014).
Frequently Asked Questions
In Blood Pressure (BP) measurements, the highest number is systolic BP, while the lower number is diastolic BP. More than 90 over 60(90/60) and less than 120 over 80 (120/80) is a normal or healthy BP
As per various research, Essential Hypertension cannot be cured. It can be controlled through various ways like medication, lifestyle modifications. Hypertensive patients need to have regular medical follow up.
If untreated, prolonged high blood pressure leads to other chronic health conditions such as heart attack, stroke, kidney diseases. These conditions may result in morbid conditions, ultimately resulting in death.
Uncontrolled hypertension results in excess strain on coronary arteries (blood vessels supplying oxygenated blood to the heart) which may result in the blockage due to the build of fat. Arteries harden ultimately resulting in a heart attack.
Various aspects of the likelihood of hypertension such as age, gender, family history, lifestyle, weight, family history.
As per literature and various research uncomplicated hypertension has no symptoms. General Signs and Symptoms are Headaches, Ringing in the ears, Unexplained dizziness, Spontaneous nosebleed, Depression without apparent cause, Blurred vision, Tension when there is no cause, Flushing of the face, Fainting spells.
There is no clear evidence that occupation is related to hypertension. Lifestyle and socioeconomic and dietary factors mostly contribute more to hypertension.
Though many studies claim that high salt intake may lead to hypertension; as there is an imbalance, sodium ultimately resulting in kidney functioning.
As it is rightly said, there is no cure for hypertension. Controlling and maintaining blood pressure through a healthy lifestyle, maintaining a healthy weight and regular self and medical monitoring can help one can tackle hypertension. Emphasizing foods rich in complex carbohydrates, balanced fat and increasing fiber in your diet can be achieved by eating lots of vegetables, grains, and fruits
About 80 percent of all high blood pressure cases may be reversed by deliberate changes in diet and lifestyle. Nearly everyone with high blood pressure can dramatically lower their blood pressure by self-monitoring and opting for a healthy lifestyle.
- James Scala, 25 Natural Ways To Control Blood Pressure; Keats Publishing, Mc Graw Hill 2002
- Hypertension: Pathophysiology And Treatment; Continuing Education In Anaesthesia, Critical Care & Pain,Volume 4:2004
- Clinical Guidelines For The Management Of Hypertension. World Health Organization Regional Office For The Eastern Mediterranean Cairo 2005
- Clinical Pharmacology of Antihypertensive Therapy for the Treatment of Hypertension in CKD; Clin J Am Soc Nephrol Vol- 14: 2019
- Medicine Update; Young Hypertensive: How and How much to Investigate? Vol. 18: 2008
- Understanding the role of genetics in hypertension; European Heart Journal Vol- 38:2017
- Gender Differences in the Regulation of Blood Pressure; Hypertension Vol-37: 2001
- Hypertension and diabetic retinopathy—what’s the story? Br J Ophthalmol Vol 83: 1999
- Hypertension and cerebrovascular disease; Seminars in Cerebrovascular Diseases and Stroke; vol-3: 2003
- Dietary Supplements In The Management Of Hypertension And Diabetes – A Review Afr J Tradit Complement Altern Med; Vol 11: 2014
- Hypertensive crises: diagnosis and management in the emergency room; European Review for Medical and Pharmacological Sciences Vol-8: 2004
- Obesity-Induced Hypertension Interaction of Neurohumoral and Renal Mechanisms; Circulation Research; Vol-116: 2015
- Hypertensive Retinopathy and Risk of Stroke; Hypertension; Vol-62: 2013.